Source: USC Viterbi School of Engineering
By Greta Harrison
Chemical engineers from the USC Viterbi School of Engineering have unlocked a fatal vulnerability in many cancer cells—sugar inflexibility.
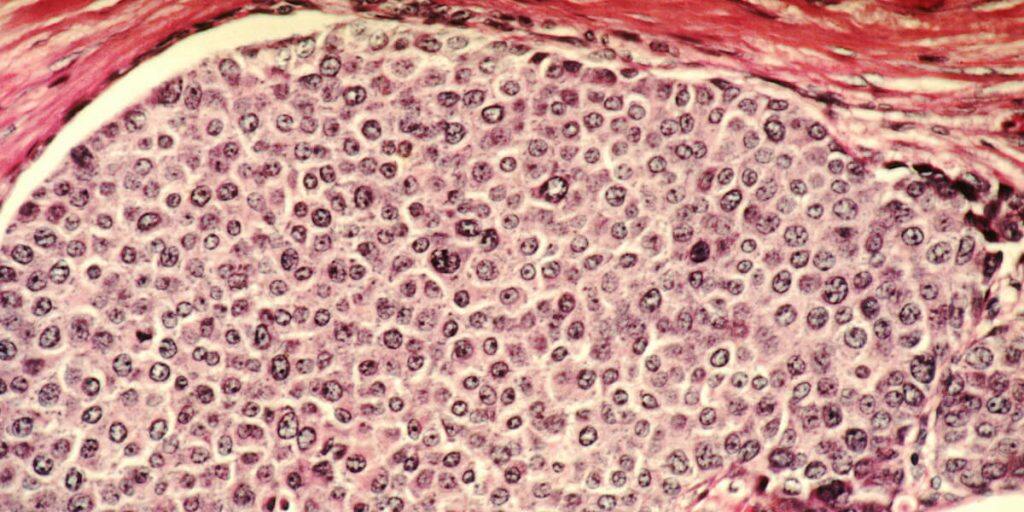
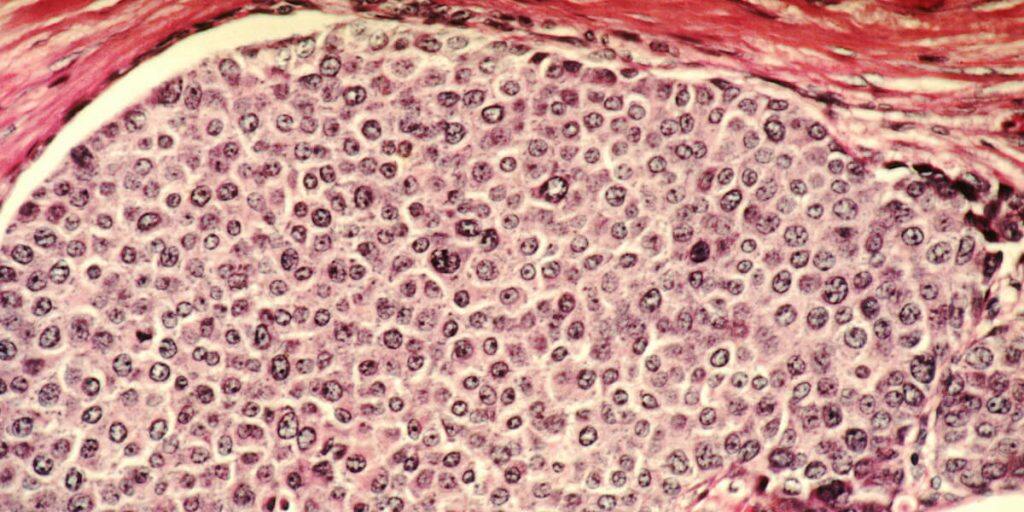
Like any cells in the body, cancer cells need sugar – namely glucose – to fuel cell proliferation and growth. Cancer cells in particular metabolize glucose at a much higher rate than normal cells. However researchers from USC Viterbi’s Mork Family Department of Chemical Engineering and Materials Science have unlocked a weakness in a common type of cancer cell: sugar inflexibility. That is, when cancer cells are exposed to a different type of sugar – galactose – the cells can’t adapt, and will die.
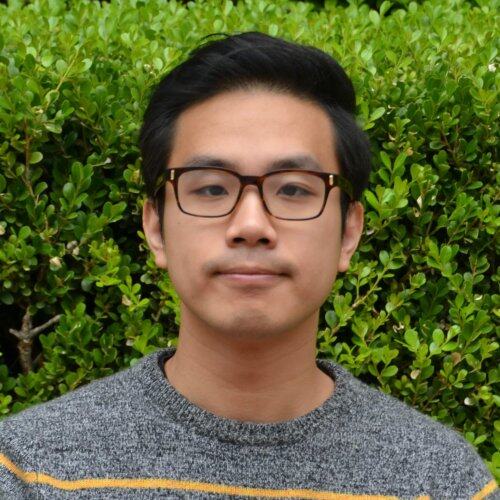
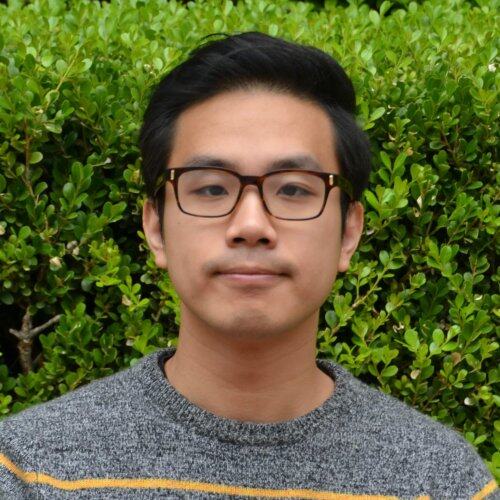
The discovery, which could have important implications for new metabolic treatments for cancer, was led by Dongqing Zheng, a PhD student in the lab of Nicholas Graham, assistant professor of chemical engineering and materials science. The research was recently published in the Journal of Cell Science.
The paper describes how oncogenes, the genes that cause cancer, can also lead cancer cells to become inflexible to changes in their sugar supply. Normally, cells grow by metabolizing glucose, but most normal cells can also grow using galactose. However, the team discovered that cells possessing a common cancer-causing gene named AKT cannot process galactose, and therefore they die when exposed to this type of sugar.
Zheng said that galactose is quite structurally similar to the glucose which helps cancer cells thrive, but that it has some differences. Graham said that exposing cells to galactose forces them to do more oxidative metabolism, where oxygen is used to convert sugars into energy, as opposed to glycolytic metabolism, where energy is derived from glucose. Normal cells can metabolize both glucose and galactose, but cancer cells that with an activated AKT signaling pathway, commonly found in breast cancer cells, cannot.
“We hadn’t seen research looking at galactose in a cancer context, to see whether specific mutations can cause cancer cause cells to be better or worse at managing that switch between glycolytic and oxidative metabolism,” Graham said.
Zheng said that the discovery did not mean that galactose itself would be an effective treatment for AKT-type cancer cells, but that it did uncover a fundamental flaw in these cells, whereby the oxidative state leads to cell death.
“What we’re trying to do is to use a systems approach to understand this, so we can use some type of targeted drug or gene therapy that can induce a similar effect and force the cell into this oxidative state,” Zheng said.
“Galactose is a model system that we’re using to uncover these vulnerabilities in cells that would then lead to future drug development,” Graham said. “Our lab will focus on trying to use drugs specifically to do that.”
The team’s findings also showed that while the oxidative process brought on by galactose did result in cell death in AKT-type cancer cells, when the cells were given a different genetic mutation, MYC, the galactose did not kill the cells.
“So if you had a drug that could inhibit glycolysis, you would give it to a patient that had an AKT mutation,” Graham said. “But you wouldn’t give it to a patient that had an MYC mutation, because it wouldn’t work theoretically for those MYC cells.”
The researchers also discovered after around 15 days in galactose, some cancer cells started to reoccur.
“Maybe there is a small sub population that are resistant to the galactose,” Zheng said. “The other possibility is that some cancer cells are very resilient and they adapt and reprogram themselves after two weeks exposed to the galactose treatment.”


The systems biology approach to cancer treatment is different to traditional treatments like chemotherapy and radiation therapy in that it targets metabolic processes in cancer cells. It aims to identify drugs without a lot of the side effects of traditional chemotherapies that also kill healthy cells, leading to adverse effects such as hair loss. However some resurgence is common in a lot of targeted metabolic treatments for cancer, which demonstrate strong initial results before a partial recurrence of the cells. Graham said that AKT tumors can potentially be targeted using a metabolic treatment like this, in order to initially shrink the tumor, but that the treatment would need to be accompanied by another treatment in a drug cocktail to prevent recurrence and protect against cancer cells mutating and adapting.
Zheng and Graham said the latest research would not have been possible without the work of undergraduate students Jonathan Sussman (biomedical engineering) and Matthew Jeon (chemical engineering and materials science), who assisted with cell counting tasks and proteomics – the study of the proteins involved in the cancer cells’ metabolism.
Graham said that moving forward, the team’s biggest challenge is to figure out which types of combination treatments to apply to test in cancer cells with the AKT gene, to lead to more effective therapeutics.
The research was funded by the Margaret E. Early Medical Research Trust, the Rose Hills Foundation, the USC Provost’s Office and the USC Viterbi School of Engineering.








































