In collaboration with the Guangdong CDC, Hunan CDC, Sun Yat-Sen University and Southeast University, Professor Yuguo Li, Chair Professor of Building Environment, and his team at the Department of Mechanical Engineering of the University of Hong Kong (HKU), conducted a series of epidemiological and environmental studies on three important Covid-19 outbreak cases in Mainland China and Tokyo, and revealed that poor air ventilation plays a key role in its spread in indoor environments.
Professor Li is an expert in ventilation of indoor environments with a focus on environmental transmission of diseases. During the SARS outbreak in 2003, Professor Li and a group of mechanical engineering experts at HKU developed an advanced mechanistic airflow model with computational fluid dynamics simulations and detailed thermo-fluid analyses to track and explain the main infection pattern and characteristics of the outbreak at Amoy Gardens and at Ward 8A of Princess of Wales Hospital.
The team studied three major outbreak cases that occurred between January and March 2020:
The Guangzhou Restaurant case (occurred on January 24, 2020) where nine members from three non-associated families sitting in three separate tables (A, B and C) were infected by an index patient at table A located in the middle. Four people in the same table, three people in table B on the left side of A, and two people in table C on the right side, were eventually infected. The three families did not know each other and had essentially no contact before, during or after the meal. The distance between the index patient (A1) and the furthest away infected patron was 4.6 metres.
The Hunan buses case (occurred on January 22, 2020) where an index patient took two buses subsequently from Changsha to his home village in an afternoon and eventually infected 10 passengers in total. first leg of the journey involved a bus with 46 other people (passengers/driver). The 3 hours 20 minutes’ ride resulted in seven passengers being infected. In the second journey on a minibus lasting about an hour, two out of 17 other people (passengers, driver and conductor) were infected. distance between the index patient (A1) and furthest away infected patron was 9.5 metres.
The Diamond Princess Cruise case in Tokyo (January to March 2020), where a total of 696 confirmed cases (552 passengers and 144 crew members, of those 410 were asymptomatic) were reported by March 5, 2020 among the 2,666 passengers undergoing quarantine in their staterooms and 1,045 crew members on board the ship.
“In both the Guangzhou Restaurant case and the Hunan buses case, there is evidence that airborne is the probable way of transmission of the virus, given that those infected were sitting at a distance, and quite a number of them more than 2m apart from the index patients, and no other transmission route can explain the spatial pattern of the infection. We found that a poor ventilation rate is a major contributing factor to the virus’ spreading in the environment.” Professor Li said.
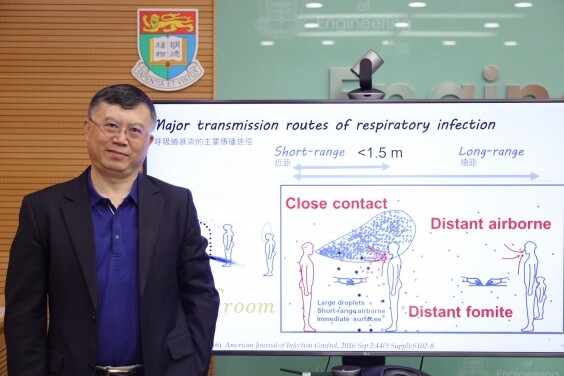
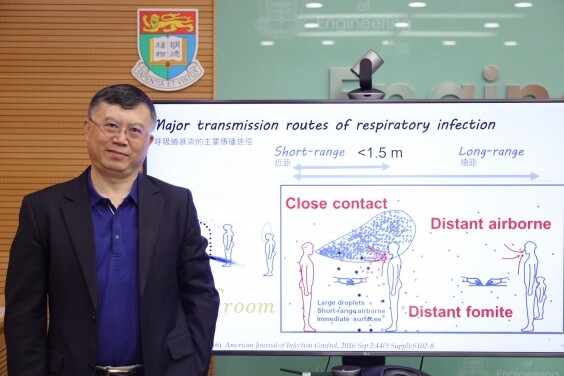
In short-range airborne transmission of diseases, droplet concentrations in the exhaled jet of air from an infected person continually decrease away from the mouth and the exhaled jet becomes sufficiently weakened to be indistinguishable from the background room air at a distance of approximately 1.5 m. However, if air ventilation is insufficient, the short-range airborne transmission route can be extended to result in a long-range airborne route to infect more people beyond the proximity (opportunistic airborne).
In the Guangzhou Restaurant case, the team in mid-March measured the ventilation rates and the restaurant’s air-conditioning, and dispersed a warm tracer gas as a surrogate of exhaled droplets from the index patient suspected [Reference 1]. Computer simulations were also performed to trace the spread of the patient’s fine exhaled droplets.
“The ventilation rate was measured to be only 1 L/s per person in the restaurant while the international standard ASHRAE 62.1 requires at least 5 L/s per person. The infection distribution is consistent with a spread pattern representative of exhaled virus-laden aerosols.” Professor Li said.
This can explain why people in the three tables got infected, despite having no contact with one another. Tracking the airflow path also revealed that the three tables A, B and C are essentially on the same air circulation loop. This also explains why none of the restaurant waiters or remaining 68 patrons at 15 other tables, which were on different circulation loops from other air-conditioning units, were infected.
Similar findings were obtained from the Hunan buses case. The team compared the airflow of the bus and the minibus in the two journeys and suggested that the difference in the ventilation rates may be a contributing factor to the risk of transmission.
The bus had a time-averaged ventilation rate of 1.7 L/s, whereas the minibus had a better time-averaged ventilation rate of 3.2 L/s per person. The infection distribution is also consistent with a spread pattern representative of exhaled virus-laden aerosols. This may explain why the infection rate at the minibus is lower.
In the Diamond Princess Cruise case, the team analysed the daily records of 197 of the 286 symptomatic infected cases (149 passengers and 48 crew) when the quarantine ended on February 19 and back-calculated their dates of infection from the epidemic curve [Reference 2]. It is found that infection among passengers after the onset of quarantine on February 6 was limited to those who stayed in the same stateroom with an infected passenger. The other cases were infected before the quarantine period. The team hence inferred from the findings that the central air conditioning system in the staterooms did not play a role in the disease’s transmission, i.e. no long-range airborne transmission route between staterooms can be identified. Although the team was unable to obtain measurements on ventilation rates of the ship during the period, the team took reference from international standard such as ISO 7547:2004, which has a requirement of 8 L/s per person, similar to the minimum ventilation rates for offices and other public spaces in ASHRAE 62.1.
Concluding from the findings (table 1), the team suggests that airborne transmission of COVID-19 outbreak in the indoor environment is likely when the ventilation rate is less than 3 L/s per person, with a sufficient exposure period. Professor Li also expects a ventilation rate of 8-10 L/s per person, similarly to that on the cruise, to be sufficient for minimizing airborne infection risk.
“Our findings do not rule out large droplets or other possible sources of Covid-19 transmission such as aerosols generated during medical procedures or fomites via contaminated surfaces. The findings instead provide evidence that short-range airborne is also a major transmission channel, which in turn suggests that other precautionary measures have to be taken in order to better contain the pandemic.” Professor Li said.
The major culprit is opportunistic airborne that occur in poorly ventilated areas, which can be understood as that a normally non-long-range-airborne infection turns to long-range airborne in poorly ventilated spaces. Opportunistic airborne transmission can lead to super-spreading events.
Professor Li said the most effective intervention to prevent the opportunistic transmission of COVID-19 is by effective ventilation and filtration and made the following recommendations:
- To enhance air ventilation in indoor environments particularly in restaurants, public transport, bars, gyms, etc.
- An indoor venue for heavy activities needs a higher ventilation rate than those for normal activities. Avoid social gatherings in an indoor environment where sufficient ventilation is not provided.
- Installation of Carbon Dioxide (CO2) sensors in a room can be useful. A concentration of over 1,000 ppm may indicate that the room is not sufficiently ventilated.
Professor Li said, “One simple criterion for insufficient ventilation is that you can smell others’ breaths even from a distance.”
In addition, the team extracted case reports of COVID-19 from the local Municipal Health Commissions of 320 non-Hubei prefectural municipalities in China by February 11, 2020 [Reference 3]. They identified all outbreaks involving three or more cases and reviewed the major characteristics of the enclosed spaces in which the outbreaks were reported. 318 outbreaks with three or more cases were identified, involving 1,245 confirmed cases in 120 prefectural cities. All identified outbreaks of three or more cases occurred in an indoor environment, which confirms that sharing indoor space is a major SARS-CoV-2 infection risk.
“Although our study does not rule out outdoor transmission of the virus, the probability of outdoor transmission however seems to be lower than indoors.” Professor Li added.






































