A new protocol for prone positioning — a technique commonly used to treat COVID-19 patients in respiratory distress by turning them on to their front to increase oxygen flow to the lungs, is published in the Journal of Frailty and Aging.
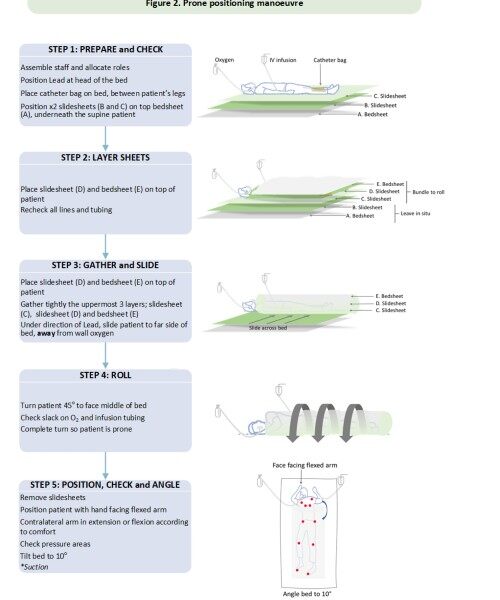
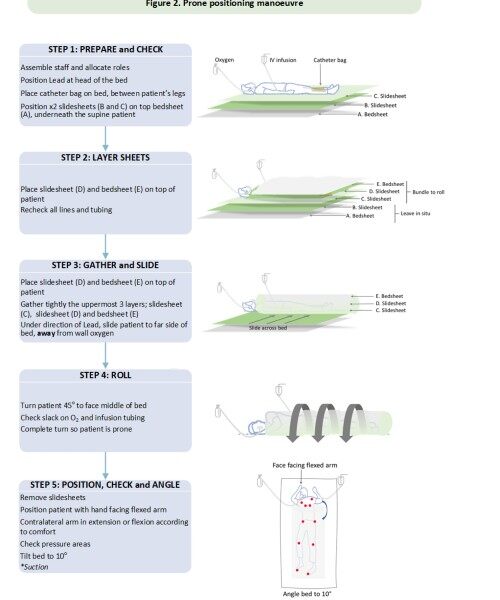
Image credit: University of Bristol
Researchers from the University of Bristol in collaboration with clinicians at the Royal United Hospital in Bath, conducted a literature review of the manoeuvre to develop a standard protocol for the adjuvant treatment that can be used for COVID-19 patients at high risk of dying being treated in normal hospital wards.
Used to relieve hypoxia (low blood oxygen) since the 1970s, proning is associated with improving outcomes in those in respiratory distress and is commonly used during anaesthesia and in patients who are intubated and ventilated. Yet despite its use over several decades, there is limited guidance for clinicians on the optimal use of the manoeuvre and requisite monitoring.
A multidisciplinary team with expertise in caring for older adults with acute COVID-19 infection and based in the Ageing and Movement Research Group in Bristol’s Population Health Sciences sought to design a means by which alternative positioning of people with severe lung infections could improve their oxygen levels. They reviewed five studies that provided details of the technique which involved patients being cared for whilst lying on their fronts. This procedure is widely used in intensive care environments, but expertise, familiarity and staffing levels often preclude its use in normal NHS ward environments.
Two of the five studies tested the protocol in patients with non-invasive ventilation, and three described a protocol but did not test it in patients. Using the data from these five articles and from relevant clinical guidelines the study showed as well as being cost effective, when patients are positioned prone their oxygenation improves dramatically. While the studies did not provide conclusive evidence to suggest a consensus on optimal duration in the COVID-19 population, studies that compared duration show a trend towards longer periods being of greater benefit.
Dr Emily Henderson, an Honorary Consultant Geriatrician at the Royal United Hospital Bath and Senior Lecturer at the University of Bristol and the study’s senior author, said: “Working on the frontline throughout the pandemic, I have sadly seen a large number of older adults in particular, die as a result of severe Covid-19 infection. Prone positioning is often used in intensive care settings and was a successful strategy that we trialled during the pandemic. We were struck by how little research there was to guide who this might benefit from this and how it could be adopted into practice safely. We are delighted to have developed a protocol for this potential adjuvant treatment. We look forward to exploring whether this, in addition to the drug treatments that are being developed and tested in large trials, may improve survival and outcomes. This strategy has particular utility for older people who are often looked after in NHS ward environments with Covid-19 infection.
Danielle Brazier, an academic physiotherapist at the University of Bristol, added: “Prone positioning for people with Covid-19 is a promising option but there’s a lot that needs to be considered prior to and during the procedure. We have designed a simple protocol to guide clinicians caring for people with Covid-19 infection. It was great to work with a multidisciplinary team of academics and clinicians to develop this guide.”