England’s salt reduction programme will have led to nearly 200,000 fewer adults developing heart disease and £1.64 billion of healthcare cost savings by 2050, according to research by Queen Mary University of London.


However, the researchers warn that the recent stalling of salt reduction programmes is endangering the potential health gains, as salt intake remains significantly higher than recommended levels.
Excess salt intake is strongly linked with raised blood pressure and increased risks of cardiovascular disease, as well as kidney disease, gastric cancer and osteoporosis. Raised blood pressure is responsible for half of the burden of ischemic heart disease and more than 60 per cent of strokes.
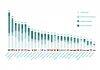
In 2003 to 2010, the Food Standards Agency, in collaboration with the food industry, established salt reduction targets in over 85 food categories, which involved reformulating processed foods, product labelling and public awareness campaigns. Consequently, average population-level salt intake reduced by 15 per cent in the period 2000 to 2011, with the decline attributed to food companies reformulating their products.
The new research, published in the journal Hypertension, used 2000-2018 population survey salt intake data and disease burden data to project the impact of the salt reduction programme, and found that:
- The 2003 to 2018 salt reduction programme in England achieved an overall salt intake reduction of 1 gram/day per adult, from 9.38 grams/day in 2000 to 8.38 grams/day in 2018.
- If 2018 salt intake levels are maintained, by 2050 the programme would have led to 193,870 fewer adults developing premature cardiovascular disease (comprising 83,140 cases of premature ischemic heart disease and 110,730 premature strokes), and £1.64 billion of health care cost savings for the adult population of England.
- If the World Health Organization recommended salt intake of 5 grams/day is achieved by 2030 in England, these benefits could double, preventing a further 213,880 premature cardiovascular disease cases and further health and social care savings to the UK government of £5.33 billion.
Lead researcher Professor Borislava Mihaylova from Queen Mary University of London said: “Our results are striking because of the large health benefits that we see with an effective government policy of reducing salt in everyday food products.
“These gains could be seriously endangered if the policy is weakened. The stalling of salt reduction efforts in the past few years is now eating away at the potential population health gains and is costing our health service dearly.
“Over the last few years, quantities of salt in diets have remained steady at levels much higher than recommended. If we can reduce our salt intake to the recommended 5g per day, we will double health benefits and healthcare savings by the year 2050.”
Professor Graham MacGregor, Professor of Cardiovascular Medicine at Queen Mary University of London and Chairman of Action on Salt said: “This study shows the enormous health benefits and cost effectiveness of the gradual reduction in salt intake in the UK that occurred between 2003-2011. Since then, the food industry has stopped reducing the excessive amounts of salt they add to our food (80 per cent of our intake) due largely to government inaction. It’s now time for Downing Street to take decisive measures in forcing the food industry to comply. If not, many more thousands of people will suffer unnecessary strokes and heart attacks.”
The authors say that the salt reduction programme in England was highly successful until 2011 because of the government pressure on industry to reduce salt content, but that this changed from 2011 to 2017 once it continued under the Department of Health as part of the Public Health Responsibility Deal. Few of the proposed actions were implemented under the Responsibility Deal and the programme failed to achieve the National Institute for Health and Clinical Excellence’s recommended salt intake targets of 6 grams/day per adult by 2015.
The food industry in the UK is still producing high-salt products in spite of strong evidence that it is technologically feasible and commercially viable to produce lower-salt products, and there is ample room for incremental reductions in their salt content, according to the researchers.
To get back on track, they say the programme will benefit from (1) a strict enforcement of salt reduction targets, for example, through legislation or financial penalties for food companies failing to comply; (2) setting more stringent salt targets; and (3) extending salt targets to the out-of-home sector, which remain lenient and lack the proper monitoring mechanisms.
Despite the high-quality data on population-level salt intake and disease burden used, the study has a number of limitations. The sample size for measuring sodium excretion from 24-hour urine collections (the most accurate way to assess salt intake) was small. There is also a lack of salt intake data in children. The long study period may present a further limitation due to the uncertainty in model parameters, assumptions on continuity of the salt reduction programme, and evolution of cardiovascular disease and salt intake trends.