Southampton clinical researchers, working as part of a UK team, have shed new light on causes of bronchiectasis, a long-term lung condition currently effecting more than 200,000 people in the UK.
People who have bronchiectasis experience a persistent cough, shortness of breath and recurring infections because their airways have become irreversibly widened. This can lead to progressive chronic lung damage. Fortunately, with improved social conditions and accessible health care, infective causes of bronchiectasis have diminished in the UK, and genetic causes such as cystic fibrosis, primary immunodeficiency and primary ciliary dyskinesia (PCD) are therefore relatively more common.
New research from the University of Southampton, University Hospital Southampton, and the Southampton Biomedical Research Centre, in collaboration with the University of Dundee, Newcastle University, Imperial College and UCL, has revealed that PCD is often underdiagnosed as a cause of bronchiectasis.
The researchers hope the study will encourage physicians and GPs to ‘Think PCD’ and investigate the underlying cause of bronchiectasis so more patients can get the treatment they need more efficiently.
Published in the European Respiratory Journal, the study used data from the UK ‘100,000 Genomes Project’, in which individuals recruited with bronchiectasis, but without clinical suspicion of PCD, were investigated to see whether PCD was underdiagnosed.
Through whole genome sequencing, pathogenic or likely pathogenic variants (the variant is responsible for causing the disease) were identified in motile ciliopathy genes in 12 per cent of individuals (17/142) confirming a diagnosis of PCD.
One individual within the study was found to have genetic variants in a gene that is known to be important for the function of non-motile cilia, CEP164.
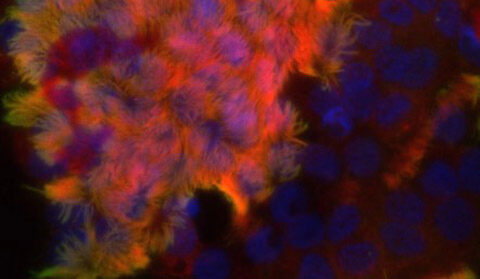
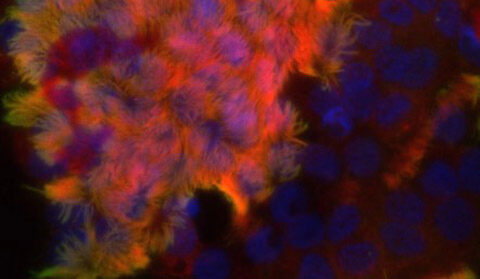
In a separate paper published in Clinical Genetics, the Southampton team, working with others, demonstrated that variants in CEP164 also effect motile cilia, which are found in the lungs and move to keep the airways clear of mucus and dirt. This was the cause of the individual’s bronchiectasis, adding to the genes known to cause PCD-like syndromes.
Jane Lucas, Professor of Paediatric Respiratory Medicine, said: “There are currently four national PCD centres in the UK – in Southampton, Leicester, Leeds and Royal Brompton London, but without a diagnosis of PCD patients do not have access to their NHS specialist multidisciplinary teams to optimally manage their disease.
“Our research highlights the need for pulmonary physicians and GPs to investigate the underlying cause of bronchiectasis. In the case of PCD, the history typically includes a daily wet cough from infancy, neonatal respiratory distress, rhinitis, glue ear and rhinosinusitis. Half of patients also have situs inversus, a rare genetic condition in which the organs in your chest and abdomen are positioned in a mirror image of normal human anatomy.
“With more genetic testing we will be able to identify bronchiectasis in more patients and ensure appropriate treatment is given to those who need it.”
Katie Dexter, from PCD Support UK, who was diagnosed with PCD in her late teens, commented: “This study confirms PCD Support UK’s concern that many with bronchiectasis have undiagnosed PCD. Without a diagnosis of PCD, individuals are likely to be excluded from accessing comprehensive specialised PCD care and risk experiencing poor long-term management of the condition.
“As a patient without heterotaxy, I did not receive a PCD diagnosis until my late teens. However, I was tested for cystic fibrosis (CF) around age 11. If CF was considered, then why not PCD? The answer is simple: my physicians were not aware of PCD.
“PCD Support UK are hopeful that this study will help raise awareness among physicians of the urgent need to ‘think PCD’ as a potential underlying cause of bronchiectasis.”








































