A new University of Alberta laboratory is working to understand how altered microbiota — fungi, bacteria and viruses in the gut and lungs — are linked with mood disorders such as depression and inflammatory immune conditions such as asthma.
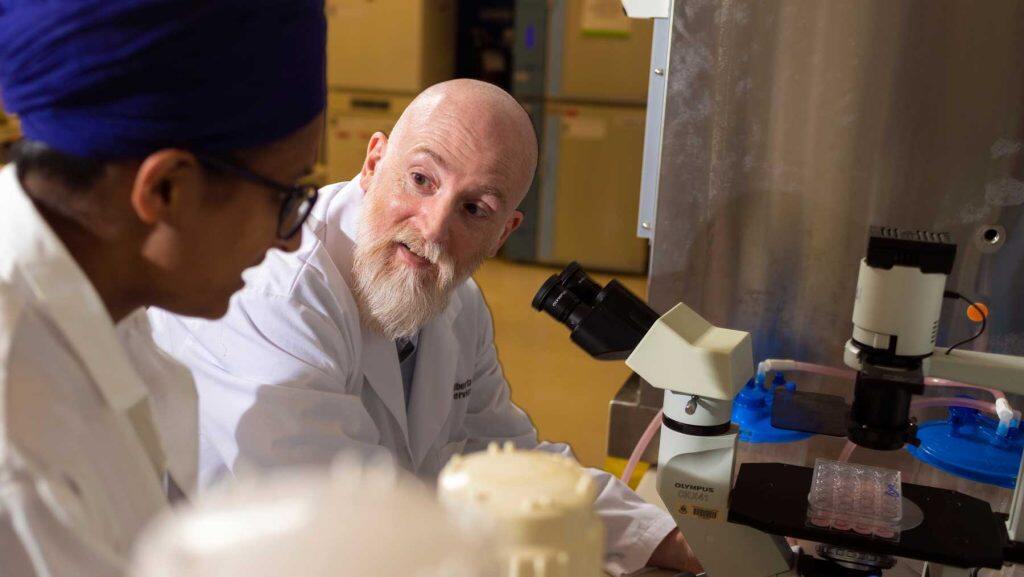
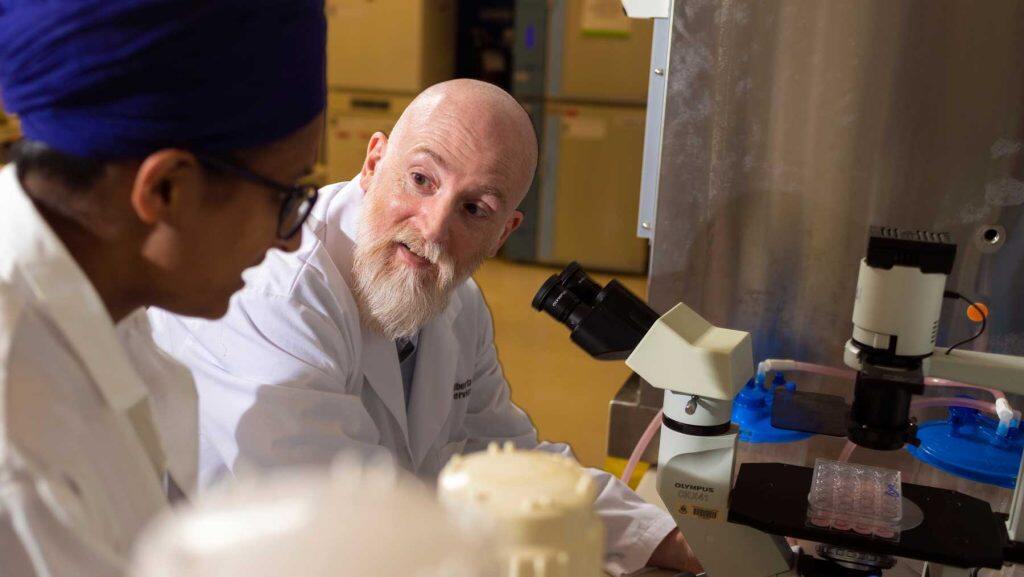
Paul Forsythe, associate professor in the Faculty of Medicine & Dentistry, was today named AstraZeneca Canada Inc. Chair in Asthma and Obstructive Lung Disease, an endowed chair that will allow Forsythe to recruit post-doctoral and graduate students and buy equipment to establish a world-leading research team.
The investment helps to ensure Alberta can attract and retain top researchers and establish the U of A as a leader in asthma and obstructive lung disease, Forsythe says. He is grateful that the biopharmaceutical company is supporting promising discovery science that could lead to new treatments.
“We know that the microbiome in early life is an important determinant of long-term health, but we don’t really understand the mechanisms going on there,” Forsythe says. “If we really want to be able to intervene therapeutically, we need to understand more. That’s what we’re doing in our lab.”
“Today’s announcement builds on our commitment to improving care and supporting leading-edge Canadian health sciences research in respiratory diseases,” says Kiersten Combs, president of AstraZeneca Canada. “We are proud to support work that promises to create meaningful advances in the treatment of asthma for patients around the world, and excited that this research is being led right here in Canada.”
“AstraZeneca’s gift is the latest in an impressive history of contributions to U of A research that spans nearly 40 years and encompasses six faculties,” says U of A president Bill Flanagan. ”This type of long-term, dedicated support plays a critical role in creating a world-class research environment. Today’s endowment of a chair in asthma and obstructive lung disease is one more example of how we are working towards finding groundbreaking solutions to the benefit of all.”
Breaking a “vicious circle”
Forsythe has spent his career examining interactions between the immune system and the nervous system in the body, usually by studying animal models.
“The two systems are often studied separately, but functionally they act together,” says Forsythe, who is also a member of the Alberta Respiratory Centre.
Rather than a cause-effect relationship, communication between the two systems is bi-directional — what Forsythe says can be a “vicious circle.” For example, psychological stress can worsen asthma symptoms, and conversely, people with asthma are more susceptible to psychological stress, anxiety and depression.
“The goal of our lab is to break that vicious circle between brain and body,” Forsythe says.
Microbiota may be altered in early life because of maternal factors or antibiotics use, which targets all bacteria, not just the harmful ones causing an ear infection or other childhood illness, Forsythe says.
That change then alters the messages sent to the brain on neural pathways from the organs, such as the vagus nerve, which controls digestion, heart rate and the immune system.
This can in turn lead to mood disorders like depression, as well as to inflammatory immune responses like asthma.
Opening the door to future treatments
Forsythe began his career at Queen’s University Belfast. He then studied at the U of A under his mentor Dean Befus, professor emeritus, previous holder of the AstraZeneca Canada Inc. Chair in Asthma and Obstructive Lung Disease and a leading expert in mast cells, which are key to the immune system. Forsythe later worked at McMaster University and will continue to collaborate with researchers there now that he has returned to the U of A.
Forsythe hopes his research into these brain-body mechanisms will open the door to future new therapies, including electroceuticals, which involve electrical stimulation of specific nerves to change the messages being sent to the brain.
He and others will also continue to study the potential benefits of microbe-based therapeutics such as probiotics. For now, Forsythe suggests giving children probiotics when they are prescribed antibiotics, which may reduce harm to their microbiota.
“Antibiotics are an essential treatment that save millions of lives, but at the same time, there are downsides and we are looking for strategies to mitigate those downsides,” Forsythe points out. “Taking a probiotic is not going to do any harm, and there is the chance that it will have a beneficial effect.”







































