University of Glasgow scientists are to receive £1.7m from Cancer Research UK to investigate both the root causes of cancer and how treatments can be improved.
Professor Stephen Tait, of the Cancer Research UK Beatson Institute and the Glasgow University School of Cancer Sciences, will receive £1,646,832 to investigate what causes cancer cells to grow out of control and form tumours.
While Dr Conchita Vens, who is based at the Wolfson Wohl Cancer Centre, will receive £99,000 to explore how to overcome cancers which are resistant to radiotherapy.
Professor Tait’s research will explore how cancer cells can cheat death by getting round the “kill switch” mechanism. This “kill switch” mechanism is a powerful way of stopping tumours from growing. Its discovery has sparked the development of a new class of anti-cancer drugs, called BH3-mimetics, which directly target this mechanism effectively in different cancers types.
However, some researchers have found that the “kill switch” mechanism can help cancer grow if the mechanism is not fully activated or if the cancer cells find a way to tell nearby cells to keep growing and so reduce the effectiveness of cancer treatments.
Professor Tait’s team will explore this possibility further in the lab to see how pancreatic and bowel cancer cells survive activation of the “kill switch” mechanism and explore a new method for removing surviving cancer cells.
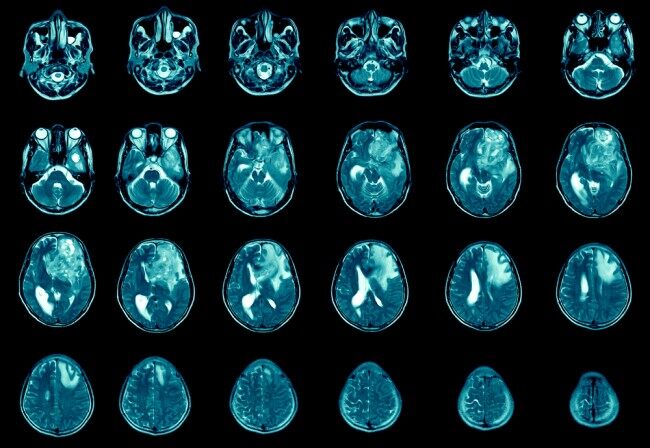
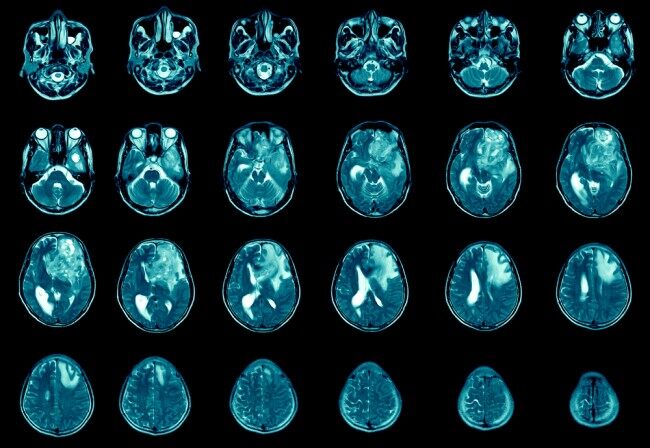
Dr Conchita Vens’ research will focus on glioblastoma, an aggressive form of cancer which mainly occurs in the brain and is currently difficult to treat. Finding new ways to tackle brain tumours is a key priority for Cancer Research UK.
In Scotland, around 32,400 people are diagnosed with cancer every year and one in two people in the UK will be diagnosed with cancer at some stage in their lives. Around 450 people are diagnosed with malignant brain tumours in Scotland every year, and every year around 390 people in Scotland die from the disease. Around one in 10 (9%) of people with a brain tumour survive for five years or more after diagnosis.
Currently, people with glioblastoma are treated with surgery, radiotherapy and chemotherapy.
Radiotherapy, combined with drugs like temozolomide, is the most common treatment option. However, not all patients can benefit from these drugs and brain tumours often return after treatment.
Dr Vens’ team, in collaboration with Professor Anthony Chalmers, will explore PARP inhibitors – a type of drug which stops cancer cells from repairing damage to their DNA caused by radiotherapy.
PARP inhibitors have been shown to make radiotherapy more effective, under certain conditions, in treating glioblastoma. However, low levels of oxygen in brain tumours can stop radiotherapy, or drugs like PARP inhibitors from working well.
To overcome this barrier, the team will combine radiotherapy with PARP inhibitors and drugs that can reverse low oxygen. They will test whether these drugs increase oxygen levels in glioblastoma and determine how effective this combination is. If successful, the team hope new drug combinations can be tested in clinical trials with the aim of improving glioblastoma treatment.
In this project, Dr Vens’ team will work with researchers in Oxford and Manchester to combine expertise and resources. Together they hope to develop a new treatment that will provide better outcomes for cancer patients.







































