Southampton researchers have created a potentially life-saving test that can quickly find out which antibiotics will and won’t work for treating a bacterial infection.


The pioneering new technique was developed by Professor Hywel Morgan at the University of Southampton and National Institute for Health and Care Research (NIHR) Southampton Biomedical Research Centre, with colleague Dr Daniel Spencer.
The diagnostic test has been spun out after a decade of research and raised £2M in a recent investment round.
It is now undergoing laboratory studies, funded by a £1M grant awarded by the NIHR i4i programme. These will run at University Hospital Southampton and Porton Down, led by the UK Health Security Agency (UKHSA).
The test gives results in a matter of hours rather than days. It could help stem the rise in hard-to-treat bacterial infections. It would allow patients’ infections to be treated before they become serious.
Prof Hywel Morgan, Professor of Bioelectronics at the University of Southampton, said: “Informed prescribing is the goal, so you can actually give the correct antibiotic for the correct bacteria, and ensure the bacteria are not resistant to that antibiotic. What it means for patients is that they get the right antibiotics earlier.
“There’s demand for faster ways of determining whether the bacteria are or are not resistant to the antibiotic you prescribe. This test takes it down from a few days to a few hours.”
Antibiotic testing
The current gold standard to find out if an antibiotic can be used to treat a bacterial infection is the disc diffusion test. A sample containing the bacteria is taken from the patient and grown in a laboratory, in a dish with a small disc infused with the antibiotic. The larger the bacteria-free space around the disc, the more effectively the antibiotic kills the bacteria. Bacteria growing right next to the disc may be resistant to the antibiotic.
This technique takes two to three days to deliver results. During this time, the patient may be prescribed an antibiotic that doesn’t work, and their infection could be getting worse. Alternatively, they may be given a broad-spectrum antibiotic, which often have bad side effects. There is an urgent need for a faster method, allowing patients to get the right treatment sooner.
Pioneering new technique
The researchers have therefore designed a new method, known as iFAST. This enables the rapid identification of antibiotic resistance within a few hours.
Just as a balloon filled with water will leak or burst when pierced, antibiotics damage the outer cell wall of bacteria to kill them. If the bacteria are resistant to the antibiotic, this will not happen. The iFAST device measures these changes to assess how effective the antibiotic will be as a treatment.
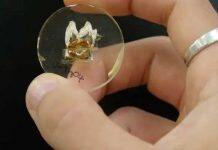
To do the test, the sample is briefly grown in the presence of antibiotics before being loaded onto a microfluidic chip. The bacteria flow, one by one, through a channel thinner than a human hair, passing between two tiny electrodes. The device uses this to measure the electrical properties of 5,000 individual bacteria in 30 seconds. This can be used to see if there is any damage to the bacteria.
The approach provides accurate data, whilst reducing the time to result by a factor of 10. This would allow doctors to rapidly prescribe an effective treatment.
Preventing bacterial resistance
Antimicrobial resistance (AMR) caused over one million deaths in 2019. This is more than malaria and AIDs combined. This a global challenge that is getting worse.
Antibiotic resistance occurs when bacteria change so that an antibiotic, or sometimes multiple antibiotics, no longer kill them. These antibiotic resistant bacteria, such as MRSA, cause infections that are much harder to treat.
AMR has many causes, including over-use of antibiotics. Rapid diagnosis and treatment of bacterial infections with the right antibiotic cuts unnecessary antibiotic use. This would help prevent antibiotic resistant bacteria spreading and increasing these hard-to-treat infections.
‘Fast-paced and exciting journey’
This iFAST investment round was led by QantX. The company received co-investment from UKI2S, KHP Ventures, Kadmos Capital, and a group of angel investors.
Dr Toby King, iFAST CEO, said: “We are delighted to welcome our new shareholders and to be able to begin the commercialisation of this game-changing technology, fighting one of the WHO’s top 10 global challenges.
“We look forward to working together on what will be a fast-paced and exciting journey, with research systems expected to be available for evaluation next year.”
David Woolley, Head of Technology Transfer and Impact Programmes at the University of Southampton, said: “iFAST Diagnostics is the latest example of University research, supported by the vibrant enterprise eco-system in place at Southampton, advancing strongly through the translational pathway to deliver real world impact.
“We’re delighted to have achieved this for the first time, in strategic partnership with the UK Health Security Agency and also having received significant NIHR funding support.
“Playing a key role in helping bring in a strong business leader in Toby King to work alongside world-leading scientists and engineers has been exciting in the last year, and I look forward to seeing iFAST continue to flourish and make a key difference in healthcare in the future.”