Researchers at the Hong Kong University of Science and Technology (HKUST) have identified new therapeutic targets for Alzheimer’s disease (AD) by studying the patients’ brain with a newly-developed methodology. This novel approach also enables researchers to measure the effects of potential drugs on AD patients, opening new directions for AD research and drug development.
Although the pathological mechanisms of AD have been studied for decades, the disease remains incurable. One reason is that conventional research approaches have limited capability to identify molecular targets for drug development. Molecular and pathological pathway analysis generally examines AD patients’ brain as a single unit, which usually underestimates the contributions of different brain cell types to AD and any abnormalities in them. This is especially the case with less-common cell types such as microglia (the brain’s resident immune cells) and neurovascular cells (specifically endothelial cells), which only account for less than 5% and 1% of the total brain cell population, respectively.


However, a team led by Prof. Nancy Ip, Vice-President for Research and Development, Director of the State Key Laboratory of Molecular Neuroscience, and Morningside Professor of Life Science at HKUST, has more than circumvented this problem––they have also identified several new potential molecular targets in endothelial cells and microglia for AD drug development.
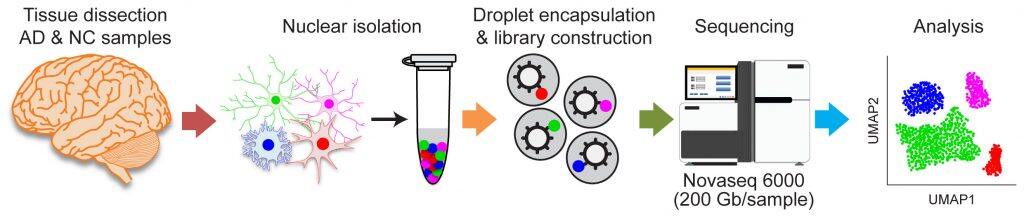
The team examined the functions of specific cell types in the postmortem brains of AD patients, which is typically impossible with conventional approaches, by using cutting-edge, single-cell transcriptome analysis, which can be used to characterize of the molecular changes in single cells. This yielded a comprehensive profile of the cell-type-specific changes in the transcriptome in the brains of AD patients. Subsequent analysis identified cell subtypes and pathological pathways associated with AD, highlighting a specific subpopulation of endothelial cells found in the brains’ blood vessels. Accordingly, the team discovered that increased angiogenesis (the formation of new blood vessels from current ones) and immune system activation in a subpopulation of endothelial cells are associated with the pathogenesis of AD, suggesting a link between the dysregulation of blood vessels and AD. The researchers also identified novel targets for restoring neural homeostasis (the ability to maintain a relatively stable internal state despite external changes) in AD patients.
The team also leveraged their single-cell transcriptome analysis to study the mechanism by which the cytokine interleukin-33 (IL-33), an important protein for immune signaling, exerts beneficial actions, making it a possible AD therapeutic intervention. The researchers found that IL-33 reduces AD-like pathology by stimulating the development of a specific subtype of microglia that helps clear amyloid-beta, a neurotoxic protein found in AD brains. The team is also the first to capture data on the mechanisms by which microglia transform into an amyloid-beta–consuming phagocytic state, which is a major cellular mechanism for the removal of pathogens.
“The complex and heterogeneous cell composition within the brain makes it difficult to study disease mechanisms,” Prof. Ip explained. “The advancement of single-cell technology has enabled us to identify specific cell subtypes and molecular targets, which is critical for developing new interventions for Alzheimer’s disease.”
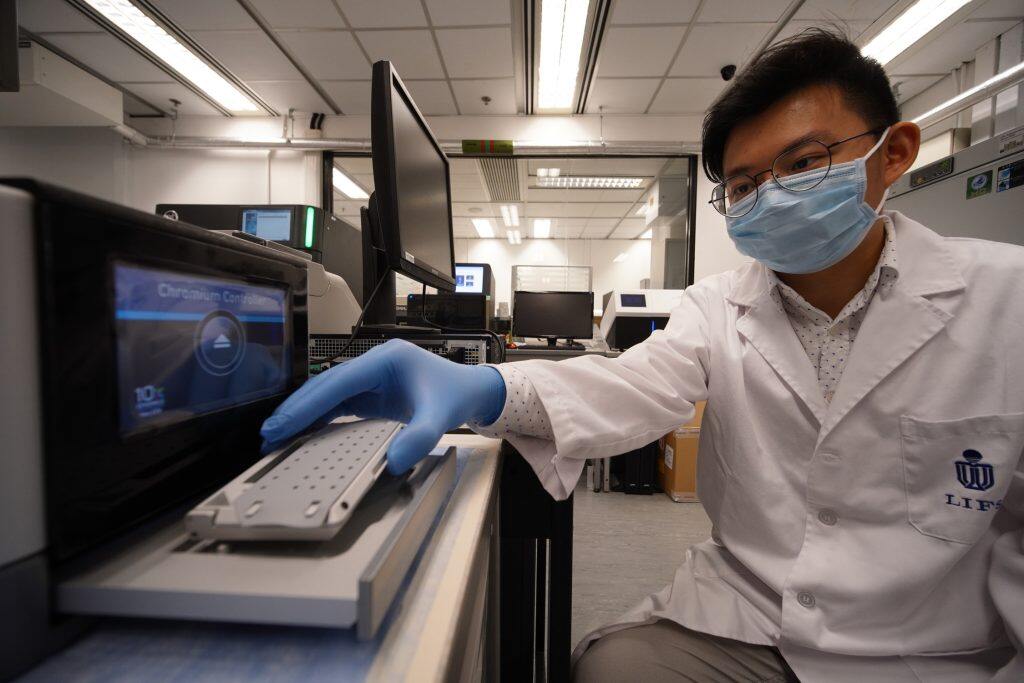
The team uses the newly-developed methodology to study AD patients brain at single cell level.
The team has recently published their work in the prestigious scientific journals Proceedings of the National Academy of Sciences U S A (PNAS) and Cell Reports.
AD, the predominant form of dementia, currently affects over 50 million individuals worldwide and is projected to afflict 150 million people by 2050. Its pathological hallmarks include the accumulation of extracellular amyloid-beta depositions and neurofibrillary tangles. Over time, ineffective clearance of these pathological hallmarks leads to cellular dysfunction in AD, resulting in memory loss, communication problems, reduced physical abilities, and eventually death.







































