A correlation exists between the weather and humidity that patients are exposed to during different stages of COVID-19 infection and the probability of death, according to Dr Sean Yuan Hsiang-yu, Assistant Professor in the Department of Biomedical Sciences at City University of Hong Kong (CityU), and PhD student Liang Jing-bo.
Using mathematical models combined with statistical analysis, the CityU team has estimated the correlation between COVID-19 case fatality rates and temperature and relative humidity based on i) the number of confirmed cases and deaths in eight European countries (UK, Italy, France, Spain, Germany, Netherlands, Sweden and Romania); and ii) data for temperature and relative humidity.
The researchers collected the data between February 2020 and July 2020, which was the first wave of the pandemic, taking into account delays in infection confirmation and death reporting, and then calculating the daily case fatality rates. Afterward, the distributed lag nonlinear model (DLNM), which was commonly used to calculate an exposure-time-response function when the exposure effect is likely to be nonlinear, was used to estimate the impacts of temperature and relative humidity on case fatality rates.
Daily relative humidity values for five countries (Italy, Spain, Germany, Netherlands, and Sweden) were collected from the European Climate Assessment and Dataset. For those countries (UK, France, Romania) lacking the relevant data, the team calculated relative humidity values using the ratio of the actual water vapour pressure divided by saturation water vapour pressure.
“Starting from the outbreak of the pandemic until July 2021, the number of deaths in Europe was over 1.11 million, which accounts for approximately 27% of total COVID-19 deaths. Although the association between weather conditions and the transmissibility of COVID-19 in Europe has been reported before, the relationship between these exposures and fatality rates has not been fully determined. Furthermore, the impact of these factors at different stages of infection on the probability of death has not been discussed yet,” Dr Yuan said.
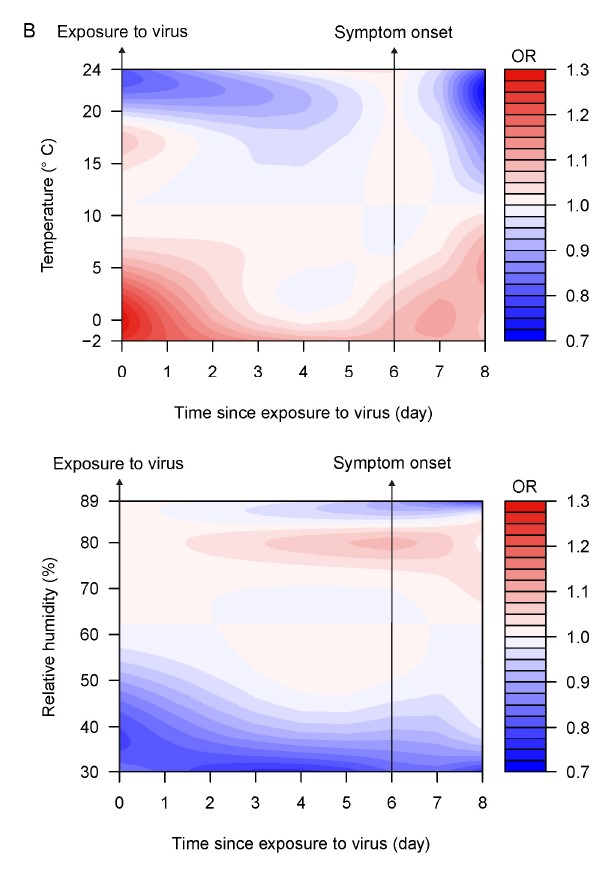
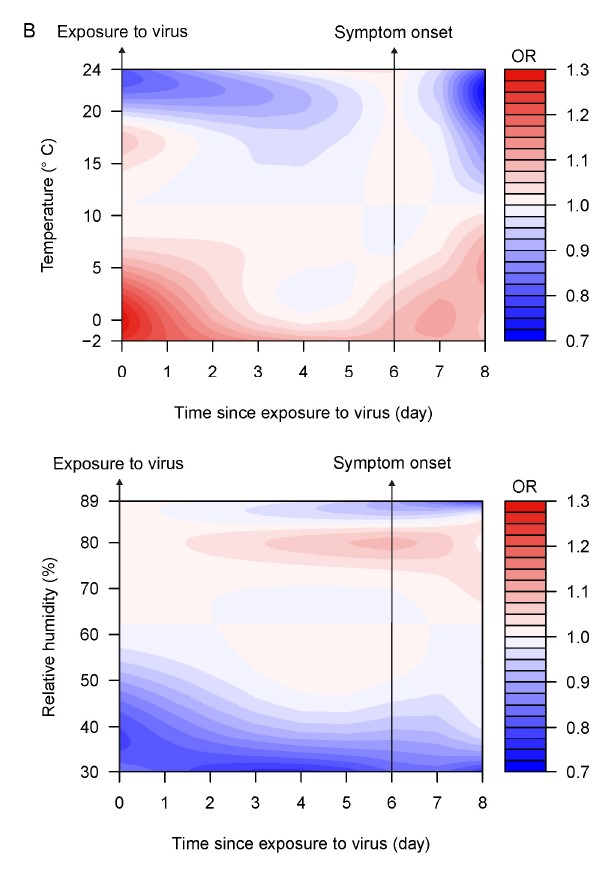
The results show that weather conditions affect fatality rates among COVID-19 cases differently, i.e. during different stages of infection. During the early stages, warmer temperatures (higher than 20°C) and low relative humidity (lower than 50%) were associated with a lower death risk; after the onset of symptoms, warmer temperatures (higher than 20°C) and high relative humidity (higher than 85%) were associated with a lower death risk. For instance, high relative humidity (89%) during the first few days after symptoms appear can reduce the fatality rate by 31%, compared to the 62% relative humidity.
So the team believes environmental conditions may affect not only the initial viral load when a person is exposed to viruses, but also how an individual’s immune system responds when symptoms start to appear. This means that avoiding the impact caused by bad weather and creating optimal indoor conditions for cases under self-isolation or quarantine may reduce the risk of death.
The team also successfully captured the statistical correlation between temperature, relative humidity and total deaths in eight European cities during the first epidemic wave. Warm conditions reduced the risk of deaths, especially when the temperature was higher than 15°C. For example, Romania showed a warmer temperature for a long period of time, while Sweden and Netherlands also showed a warmer temperature for several days. The risk of death was low when the relative humidity was below 50% as well, such as in Germany and Romania, which both had humidity below 50% for a longer period of time, which may explain why these countries experienced lower mortality rates.
“The weather in Hong Kong has been extreme recently. In addition to symptoms such as shortness of breath, fever and sore throat, patients are affected by cold weather. By studying the data in Europe, we found that temperature and humidity are closely related to fatality rates for COVID-19 cases. This study aims to provide effective recommendations to improve environmental conditions during self-isolation or quarantine after patients develop symptoms, and hence reduce fatalities,” Dr Yuan said.
He suggested that:
- patients wear warm clothing, drink more warm water, and use heaters, etc.;
- after symptoms appear, patients wear a mask as appropriate, or use a humidifier, etc., to inhale more warm and humid air; and
- government departments and/or social welfare organisations step up the distribution of materials for keeping warm to those in need.
Additionally, Dr Yuan suggested scholars conduct epidemiological observational studies in order to determine the best indoor environmental conditions for patients who are isolated at home or hospital.
As early as January 2020, at the beginning of the outbreak of COVID-19, he had already published several studies on estimating infection figures in Hong Kong using mathematical modeling combined with epidemiology studies. His research has provided public health with expert opinion. Last month, using a mathematical model that combines age-specific susceptibility to COVID-19 infections and social contact data, among others, he estimated that if social mobility decreases by around 25% when compared to the level during the Christmas and New Year holidays, a fifth wave will cause around 250,000 infected cases. That figure is similar to the current pandemic trend in Hong Kong.